 |
 |
| Organoid > Volume 2; 2022 > Article |
|
Abstract
Background
Methods
NOTES
Funding
This work was supported by the National Research Foundation (NRF) funded by the Korean government (MSIT) (2020R1A2C2010712, 2020R1A5A8019180), the Ministry of Education (MOE) (Regional Innovation Strategy (RIS)(2022RIS-005) and the National Institute of Environment Research (NIER) (2020-01-02-087).
Fig. 1.
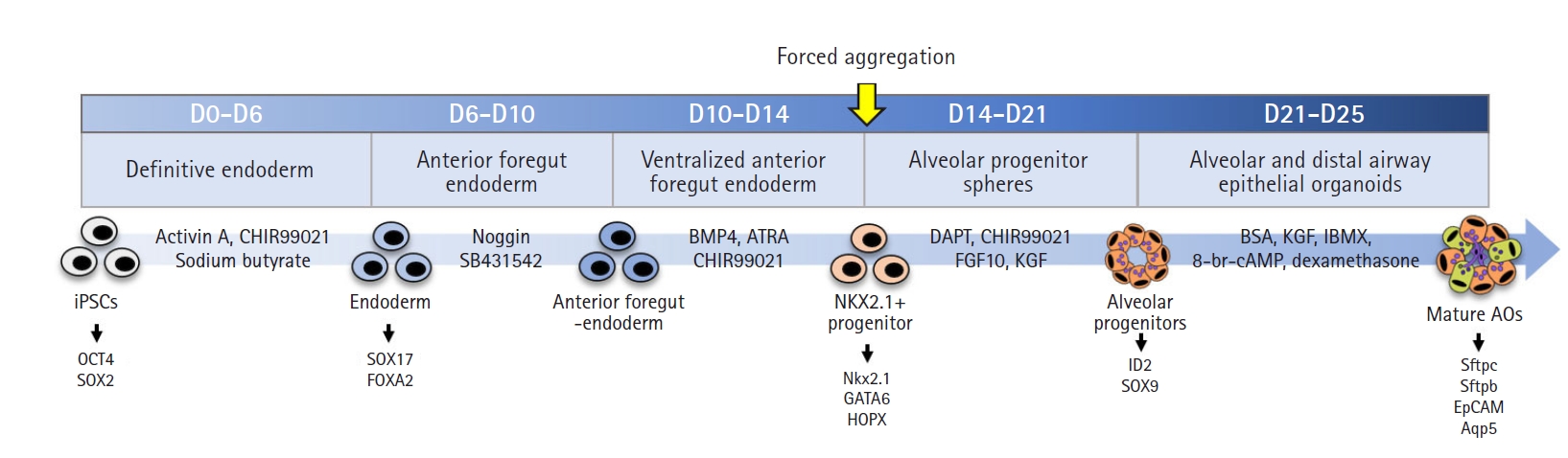
Fig. 2.
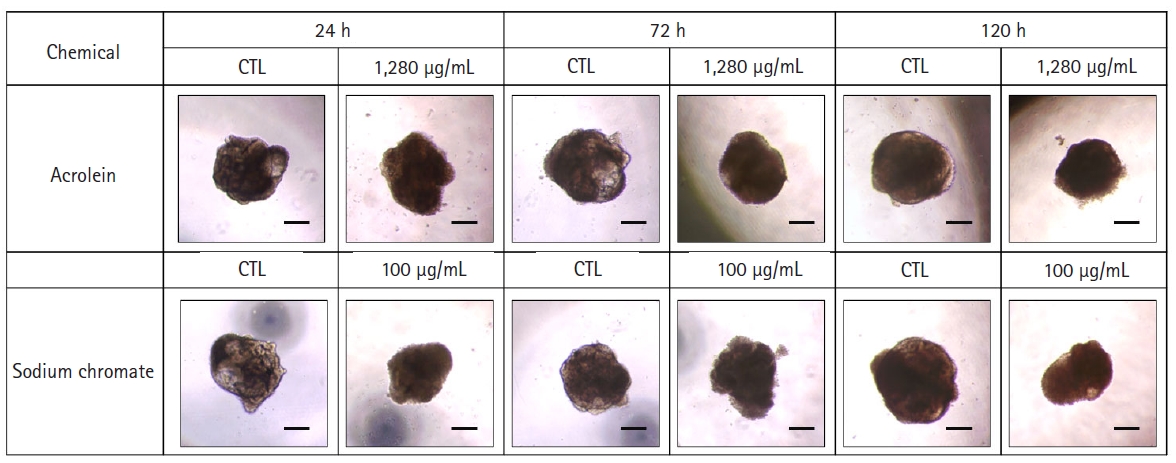
Fig. 3.

Fig. 4.

References
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,775 View
- 34 Download
- ORCID iDs
-
Jooyeon Lee

https://orcid.org/0000-0002-4681-7046Hyosin Baek

https://orcid.org/0000-0003-0276-5149Seok-Ho Hong

https://orcid.org/0000-0003-3372-442XJong-Hee Lee

https://orcid.org/0000-0002-8619-1383Seung-Jun Wang

https://orcid.org/0000-0002-6138-3952Ji Young Lee

https://orcid.org/0000-0003-4913-5654Myung Ha Song

https://orcid.org/0000-0002-5918-8410Se-Ran Yang

https://orcid.org/0000-0002-2422-213X - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



