 |
 |
| Organoid > Volume 3; 2023 > Article |
|
Abstract
NOTES
Fig. 1.
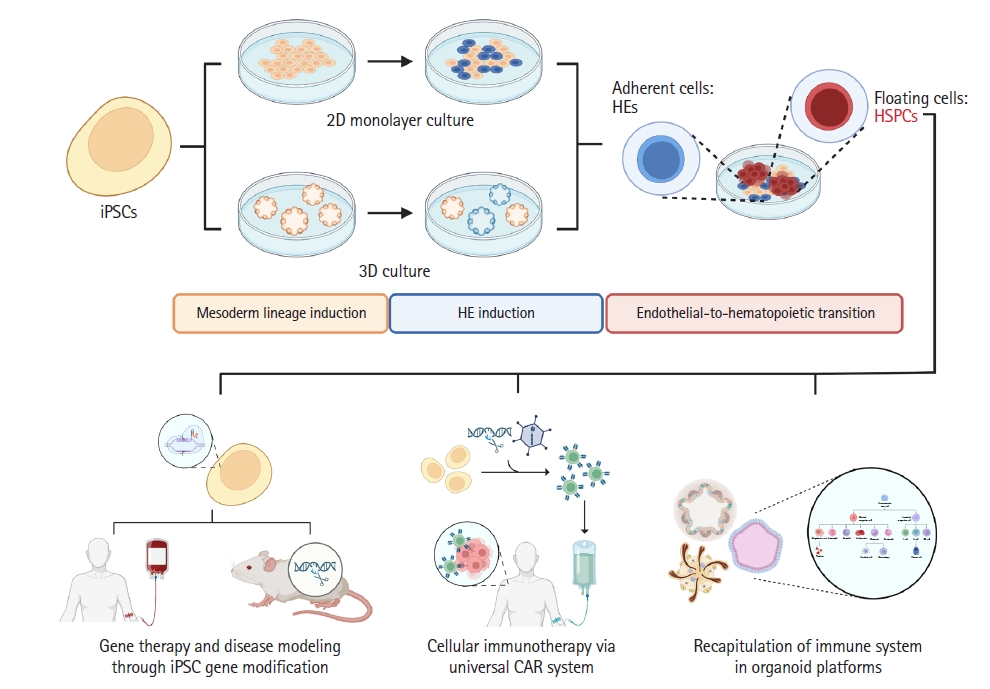
Table 1.
| Cell source | Approach | Production yield | CFU assay | Multilineage potential | Reference | |
|---|---|---|---|---|---|---|
| 2D | PBMC-derived hiPSCs | Feeder- and serum-free monolayer induction | - CD34+CD45+ HSPCs (36.5%) | BFU-E, CFU-E | Adult-type erythrocytes expressing the HBB gene and adult β, γ globin | Leung et al., 2018 [57] |
| CHIR99021 | CFU-GM/G/M | |||||
| CH-223191 | ||||||
| hESCs | Feeder- and serum-free monolayer induction | - CD144-CD43+ HSPCs (59.8%) | BFU-E, CFU-E | CD4/CD8+ T cells (84.7%) | Uenishi et al., 2018 [58] | |
| BM/CB-derived hiPSCs | DLL1-Fc | CFU-GM/G/M | Erythrocytes with increased ratio of adult-type globin | |||
| SB431542 | CFU-GEMM | |||||
| PB-derived hiPSCs | Monolayer induction | CD43+CD45+ HSPCs (56.0%) | BFU-E, CFU-E | Mature erythrocytes with adult β globin (11.1+/-2.1%). | Ruiz et al., 2019 [54] | |
| CHIR99021 | CFU-GM/G/M | |||||
| SB431542 | ||||||
| Skin fibroblast/T cell/PB mononuclear cells-derived hiPSCs | Feeder- and serum-free monolayer induction | CD34+CD43+ HSPCs (54.1%) | BFU-E, CFU-E | CD8+ T cells (76.2%) | Netsrithong et al., 2020 [55] | |
| CHIR99021 | CFU-GM/G/M | Mature GPA+ (94.8%) /Band 3+ (98.4%) erythrocytes expressing low adult globin (0.8%). | ||||
| SB431542 | CFU-GEMM | |||||
| hPSCs | Feeder- and serum-free monolayer induction | CD43+CD45+ HSPCs (41.6%) | BFU-E, CFU-E | CD4+ T cells (25.2%) | Chang et al., 2022 [56] | |
| CHIR99021 | CFU-GM/G/M | Functional CD56+ NK cells (85.3%). | ||||
| SB431542 | CFU-GEMM | |||||
| 3D | hESCs | EB induction | CD144-CD45+ HSPCs (55.0%) | EryP-CFC | CD56+CD11βlow NK cells (47%) | Sturgeon et al., 2014 [59] |
| MSC-derived hiPSCs | CHIR99021 | CD7+CD5+ (22.0%) and CD4+CD8+ (91%) T cells | ||||
| SB431542 | ||||||
| hESCs | EB induction | CD45+ blood cells (14.5%) | N/A | GLY-A+ erythrocytes | Sugimura et al., 2017 [66] | |
| PB/MSC-derived hiPSCs | CHIR99021 | CD33+ myeloid cells | ||||
| SB431542 | CD19+ B cells (84.3%) | |||||
| 7 transcription factors (ERG, HOXA5, HOXA9, HOXA10, LCOR, RUNX1, SPI1) transduction | CD3+ T cells (7.5%) | |||||
| hESCs | EB induction | CD34+CD45+ HSPCs (36.7%) | BFU-E, CFU-E | CD56+ CD45+ CD94+ CD117- LFA1+NK cells (37+/-2.92%) | Angelos et al., 2017 [60] | |
| CD34+ umbilical cord (UCB)-derived hiPSCs | SR-1 | CFU-GM/G/M | ||||
| PB-mobilized HSPCs/mononuclear cells-derived hiPSCs | Feeder- and xeno-free EB induction | CD34+CD45+ HSPCs (86.6%) | BFU-E, CFU-E | CD235a+ (4.58%)/CD71+ (0.1%) erythroid cells | Tan et al., 2018 [68] | |
| SB431542 | CFU-GM/G/M | CD33+ myeloid cells (32.7%) | ||||
| transcription factor (MLL-AF4) transduction | CD19+ B cells (60.5%) | |||||
| CD3+ T cells (1%) | ||||||
| hESCs | Organoid system | CD34+ CD43+ CD45+/- HSPCs | N/A | Naïve CD3+CD8αβ+ to conventional CD3+CD4+ T cells with diverse a T cell receptor (TCR) repertoire. | Montel-Hagen et al., 2019 [64] | |
| Fibroblast-derived hiPSCs | SB431542 | |||||
| hESCs | Serum-free ES/iPS-sac system | CD34+CD38-CD90+CD45RA-CD49f+ HSPCs | N/A | Mature GPA+CD71-erythrocytes (20%) that express adult β globin (4%) | Haro-Mora et al., 2020 [62] | |
| BM stromal cell-derived hiPSCs | ||||||
| hESCs | EB induction and OP9-DLL1 / DLL4 coculture | CD34+CD45+ HSPCs (37.0%) | N/A | CD7+ (93.6%) CD4+ (8.3%)/CD8+ (17.6%) T cells | Flippe et al., 2020 [61] | |
| T cell / fibroblast-derived hiPSCs | CD56+ NK cells (20-30%) | |||||
| hESCs | Swirler culture (bulk cell-aggregation of EB) and air-liquid interface culture | CD34+CD45+ HSPCs (15%) | Myeloid and erythroid colonies | CD3+CD4+CD8+ T cells (40%) | Motazedian et al., 2020 [63] | |
| hiPSCs | CHIR99021 | CD56+CD7+ NK cells (27%) | ||||
| SB431542 | CD19+ B cells (0.5%) | |||||
| CD34+-derived hiPSCs | Hemanoid system and OP9-DLL1/DLL4 coculture | CD43+CD45+ HSPCs (68.3%) | BFU-E | CD14+CD163+ macrophages | Ackermann et al., 2021 [16] | |
| IL-3 | CFU-GM | CD66β+CD16+ granulocytes | ||||
| CFU-GEMM | ||||||
| hiPSCs | Yolk sac-like organoid system and stirred suspension bioreactor culture | CD34+CD43+ HSPCs (14.3%) | CFU-E | CD71+GPA+ erythroblasts (33%) and CD71-GPA+ mature erythroid cells (15.8%) expressing fetal γ globin | Tamaoki et al., 2021 [65] | |
| CFU-GM/G/M | CD11b+ CD13+ CD14+ CD16+ CD33+ macrophages with normal phagocyte activities | |||||
| Mature CD4+CD8+ T cells (22.5%) | ||||||
| hESCs | Combined EB induction and 2D HE culture | CD34+CD45+ HSPCs (58.1%) | BFU-E, CFU-E | CD45+ CD56+ NK cells (50%) | Shim et al., 2022 [67] | |
| hiPSCs | HDAC | CFU-GM/G/M | ||||
| CFU-GEMM |
HSPC, hematopoietic stem and progenitor cell; PBMC, peripheral blood mononuclear cell; hiPSC, human induced pluripotent stem cell; hESC, human embryonic stem cell; hPSC, human pluripotent stem cell; NK, natural killer; MSC, mesenchymal stem cell; HE, hemogenic endothelium; EB, embryoid body; BM, bone marrow; CB, cord blood; PB, peripheral blood; UCB, umbilical cord blood; 2D, 2-dimensional; 3D, 3-dimensional; CFU, colony forming unit; BFU-E, burst forming unit-erythroid; CFU-E, colony forming unit-erythroid; CFU-GM, colony forming unit-granulocyte/macrophage; CFU-G, colony forming unit-granulocyte; CFU-M, colony forming unit-macrophage; CFU-GEMM, colony forming unit-granulocyte/erythrocyte/monocyte/megakaryocyte; EryP-CFC, primitive erythroid-colony forming progenitor; TCR, T cell receptor; GPA, glycophorin A; CD, cluster of differentiation; HBB, hemoglobin subunit beta.
References
- TOOLS
-
METRICS

-
- 1 Crossref
- 0 Scopus
- 3,842 View
- 195 Download
- ORCID iDs
-
Myoung Hee Han

https://orcid.org/0000-0002-2753-3312Da-Hyun Kim

https://orcid.org/0000-0002-6925-0951Kyung-Rok Yu

https://orcid.org/0000-0002-4685-3223 - Related articles
-
Technical advances in pluripotent stem cell-derived and tumorigenic organoids2022 ;2()


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



