 |
 |
| Organoid > Volume 4; 2024 > Article |
|
Abstract
NOTES
Funding
This work was funded by a grant from the National Research Foundation of Korea (NRF) grant (2020R1A2C200652811) and Korea Environment Industry & Technology Institute (KEITI) through -Core Technology Development Project for Environmental Diseases Prevention and Management Program, funded by Korea Ministry of Environment (MOE) (2021003310006).
Acknowledgments
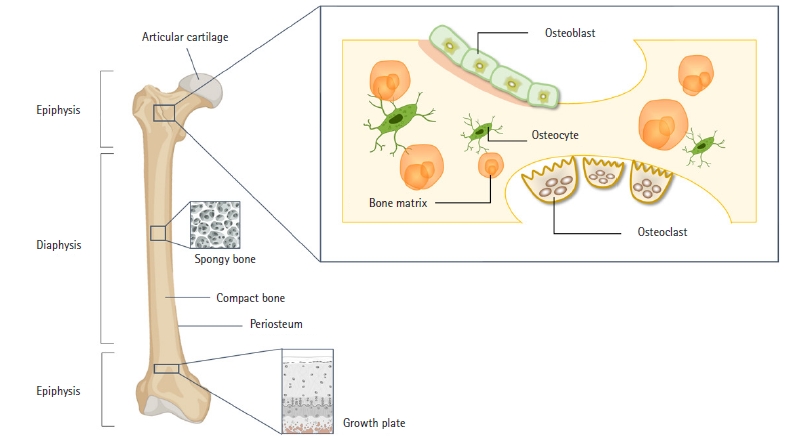
Fig. 2.
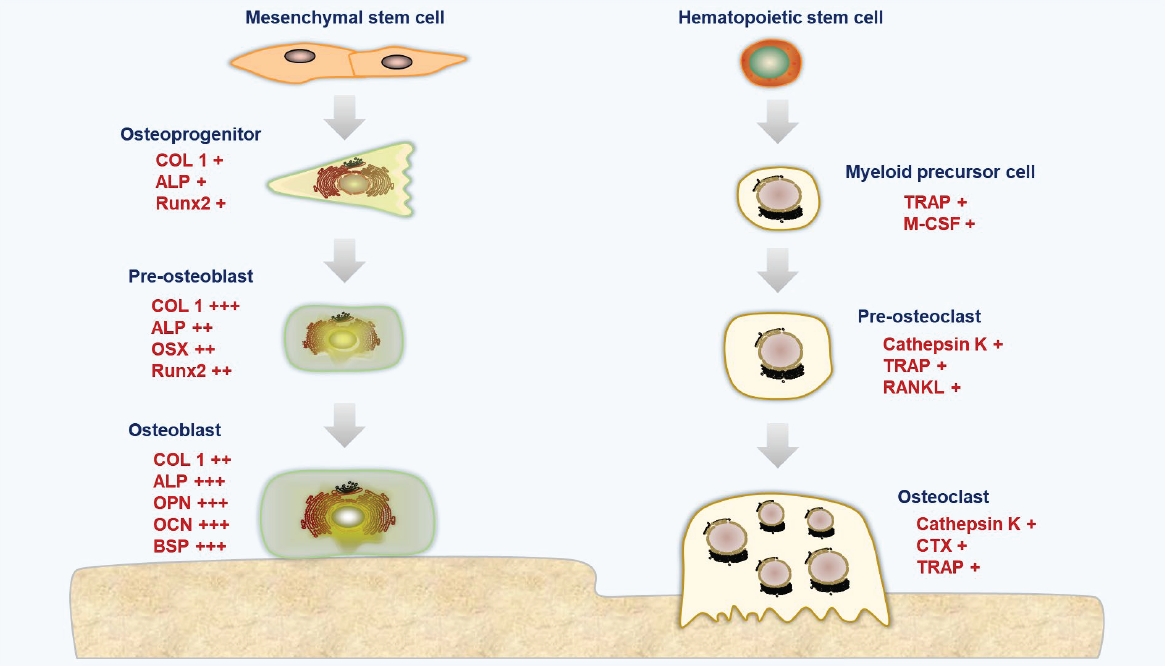
Fig. 3.
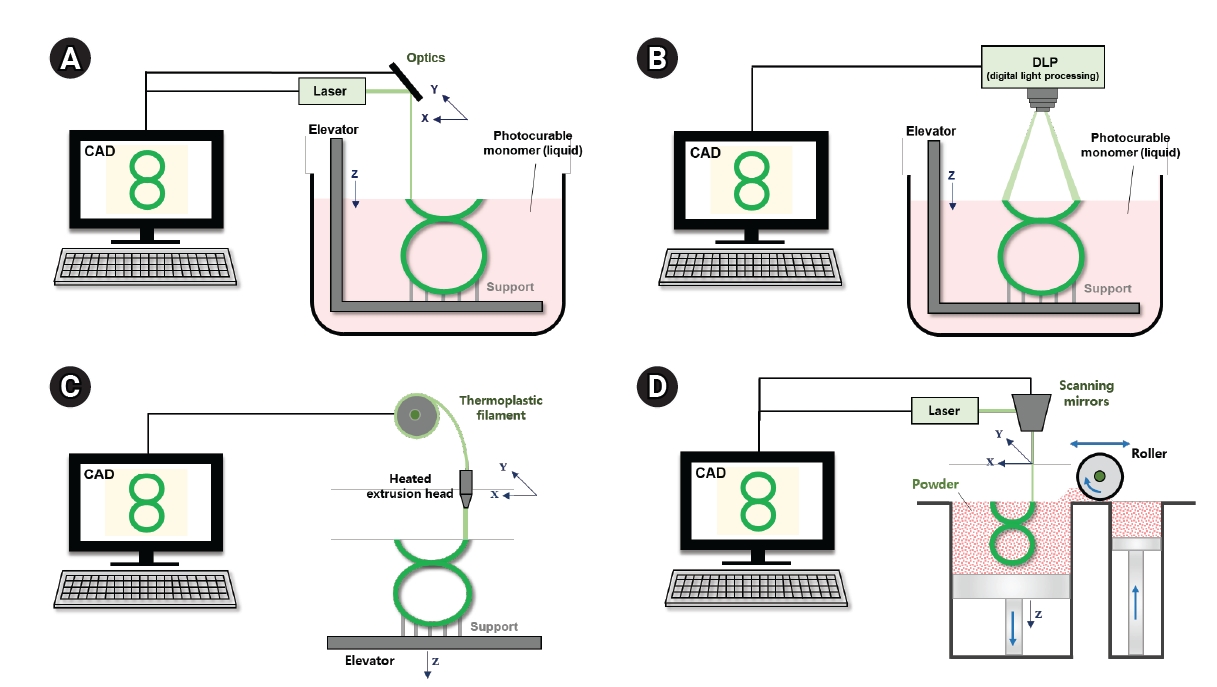
Table 1.
| Material | Cell | Finding | Ref. |
|---|---|---|---|
| β-TCP | hMSCs | Superior MSC differentiation was shown by 100 M and 7,415 scaffolds with the addition β-TCP in vitro via improved alkaline phosphatase activity and mineralized matrix formation. | [40] |
| HB ink | C3H10T12, HBOs | When SPIONs were added to HB bioink, bone grafts displayed improved bacteriostatic characteristics without cytotoxicity. | [48] |
| PCL, SrHA | rBMSCs | Significant osteogenic activity was shown by the PCL/SrHA scaffold both in vitro and in vivo. | [41] |
| PCL | hASCs | The electrospun/3D-printed scaffolds with gelatin had much higher cell proliferation than the scaffolds without it, according to cytocompatibility. | [45] |
| PLA, Ti64 | MSCs | The adhesion, proliferation, and differentiation of MSCs in Wharton’s jelly significantly improved due to the excellent effects of plasma therapy and Ti64 addition. | [44] |
| PLA, BG | MC3T3E1 | The incorporation of PLA-BG filaments was verified, as well as the scaffold’s bioactivity and cytocompatibility were confirmed. | [49] |
| PLA | SAOS-2 | The microporous architecture and osteoblast-like cell adhesion, proliferation, and differentiation were supported by 3D-printed scaffolds, simulating the natural bone hierarchical structure and promoting higher bioactivity. | [50] |
| β-TCP, HAp, CaSiO3 | mBMSCs, HUVECs | The adhesion and osteogenic differentiation of mBMSCs, as well as the angiogenic gene expression of HUVECs were encouraged by the micro/nano-HA surface layer. | [42] |
| PCL, Zn | MC3T3E1 | By triggering the Wnt/β-catenin and NF-κB signaling pathways, Zn2+ controlled osteogenesis and osteoclastogenesis. | [43] |
| PCL, HA, COL | hADSCs | The 3-component 3D-printed scaffold is a potential option for regenerating and replacing bone tissue. | [46] |
| BG, SA | rBMSCs | BMSCs preferred the BG/SA scaffolds, particularly BG/SA 2:4. These scaffolds allowed BMSCs to distribute, attach, and differentiate osteogenically. | [47] |
3D, 3-dimensional; β-TCP, β-tricalcium phosphate; hMSC, human mesenchymal stem cell; HB, hyperelastic bone; SPION, superparamagnetic iron oxide nanoparticle; PCL, polycaprolactone; SrHA, strontium-containing hydroxyapatite; PLA, polylactic acid; BG, bioactive glass; MSC, mesenchymal stem cell; HA, hydroxyapatite; COL, collagen; SA, sodium alginate.
References
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 183 View
- 3 Download
- ORCID iDs
-
Seung Yeon Lee

https://orcid.org/0000-0001-8076-6513Jin Woo Lee

https://orcid.org/0000-0003-4245-9381 - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



